Did you know that nearly 6% of the estimated 130 million people visiting US emergency rooms each year are misdiagnosed, as per the SEMrush 2023 Study? This alarming statistic highlights the crucial need to understand emergency room malpractice lawsuits. When it comes to choosing the right legal path, it’s "Premium vs Counterfeit Models" of attorneys. With a best price guarantee and free consultation included, act now! Leading US legal authorities like FindLaw and Justia recommend seeking expert advice promptly. Don’t miss out on your chance to seek justice!
General information about emergency room malpractice lawsuits
A startling fact from a new study reveals that nearly 6% of the estimated 130 million people visiting US emergency rooms each year are misdiagnosed, equating to about 1 in 18 patients getting an incorrect diagnosis (SEMrush 2023 Study). This high frequency underscores the importance of understanding emergency room malpractice lawsuits.
Types of malpractice cases
Misdiagnosis
Acute myocardial infarction (AMI) as frequently missed diagnosis
Acute myocardial infarction is one of the most commonly missed diagnoses in emergency rooms. Due to its potentially life – threatening nature, a missed AMI diagnosis can have severe consequences for patients. For example, a patient presenting with vague chest pain might be misdiagnosed with indigestion, only to later suffer a major heart attack.
High – pressure environment and time constraints
Emergency rooms are high – pressure environments where medical staff often have to make quick decisions. Time constraints can lead to hasty evaluations, increasing the risk of misdiagnosis. For instance, during a busy night shift with a high influx of patients, a doctor may not have enough time to conduct a thorough examination.
Complexity of symptoms
Many medical conditions present with complex or overlapping symptoms. This makes it challenging for doctors to accurately diagnose a patient. For example, stroke symptoms can be similar to those of other neurological disorders, leading to misdiagnosis.
Cognitive factors
Per SEMrush 2023 Study, previous studies have suggested that diagnostic errors occur in 0.6 – 12% of the patients in the emergency room, and one or more cognitive factors are related in 96% of these cases.
- Overconfidence bias: Doctors may be overconfident in their initial diagnosis and not consider alternative possibilities. For example, if a doctor has diagnosed many cases of a particular condition, they may assume a new patient has the same without further investigation.
- Confirmation bias: Doctors may look for evidence that confirms their initial diagnosis and ignore contradictory evidence. Suppose a doctor suspects a patient has pneumonia based on a cough, and then only focuses on symptoms that support this diagnosis, overlooking other possible causes.
- Availability bias: An emergency physician diagnoses three patients in a row with acute coronary syndrome so assumes that the fourth patient with chest pain is unlikely to have acute coronary syndrome (As recommended by medical training tools).
- Anchoring bias: Doctors may rely too heavily on the first piece of information they receive. For example, if a patient says they have a headache and the doctor immediately assumes it’s a common migraine, without considering other potential causes.
Communication and coordination issues
Poor communication between doctors, nurses, and other medical staff can also lead to misdiagnosis. For example, if a nurse fails to accurately relay a patient’s medical history to the doctor, it can result in an incorrect diagnosis.
Failures in clinical assessment, reasoning, or decision – making
Sometimes, errors occur due to a failure in the clinical assessment process. This could involve improper use of diagnostic tests or misinterpretation of test results.
Misdiagnosis and its consequences
Misdiagnosis is a significant issue in ER settings due to its high frequency and severity. It can lead to delayed or inappropriate treatment, which in turn can cause patients to suffer further harm, long – term disabilities, or even death.
Delayed treatment
Delayed treatment can occur for various reasons, such as waiting too long for test results, staff shortages, or administrative issues. For example, if a patient with a broken bone has to wait hours for an X – ray and subsequent treatment, it can lead to more pain and a longer recovery time.
Communication – related errors
Communication breakdowns within the emergency room can lead to malpractice. This includes miscommunication between medical staff about a patient’s condition, allergies, or treatment plan. A miscommunication about a patient’s drug allergy could lead to the administration of a harmful medication.
Elements to prove in court
Essentially, four elements must be proved to establish negligence:
- Duty of Care: The plaintiff must show that the defendant owed a duty of care to the plaintiff. This means there was a legal obligation for the defendant to avoid causing harm.
- Breach of Duty: The plaintiff must prove that the defendant breached their duty of care.
- Causation: The plaintiff has to show that the breach of duty caused the injury.
- Damages: The plaintiff must demonstrate that they suffered actual damages as a result of the injury.
Pro Tip: If you believe you have a malpractice case, start gathering evidence such as medical records, test results, and witness statements as soon as possible.

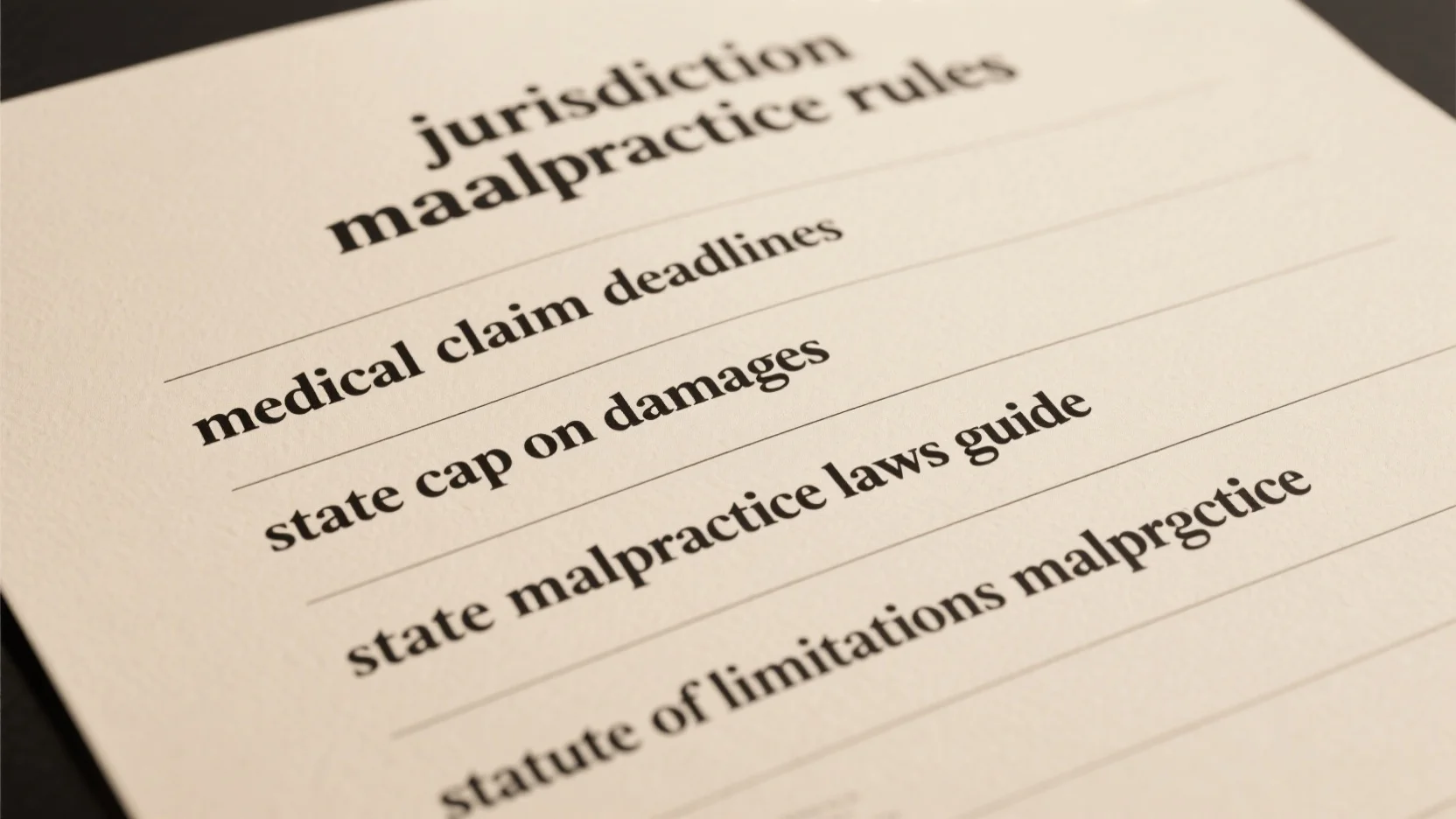
Statute of limitations
The statute of limitations for medical malpractice lawsuits varies by state. For example, in Maryland, it is five (5) years, while some states may have shorter or longer timeframes. It’s crucial to understand the statute of limitations in your state because once the time limit expires, you may lose the right to file a lawsuit. Try our legal timeline calculator to understand your state’s statute of limitations better.
Key Takeaways:
- Misdiagnosis in emergency rooms is a common issue due to factors like high – pressure environments, complex symptoms, and cognitive biases.
- To win a malpractice lawsuit, four elements (duty of care, breach of duty, causation, and damages) must be proved.
- The statute of limitations for malpractice lawsuits varies by state and is an important factor to consider.
FAQ
What is an emergency room malpractice lawsuit?
An emergency room malpractice lawsuit is a legal claim filed when a patient believes they’ve suffered harm due to negligence in an ER. This can stem from misdiagnosis, delayed treatment, or communication – related errors. Proving such a case requires demonstrating duty of care, breach of duty, causation, and damages. Detailed in our [Elements to prove in court] analysis.
How to file an ER misdiagnosis suit?
According to legal best practices, the first step is gathering evidence like medical records, test results, and witness statements. Next, consult an emergency room malpractice attorney to assess the case’s viability. Then, file the lawsuit within the state’s statute of limitations. Unlike general lawsuits, ER misdiagnosis suits require medical expertise.
Steps for a triage negligence claim
First, document all details of the incident, including time, symptoms reported, and actions taken. As recommended by legal experts, seek legal advice from a professional well – versed in emergency department litigation. After that, work with your attorney to prove duty of care, breach, causation, and damages. Detailed in our [Elements to prove in court] section.
ER error lawsuit vs general malpractice lawsuit
An ER error lawsuit is a subset of general malpractice lawsuits. Unlike general cases, ER lawsuits often involve high – pressure environments, quick decision – making, and time constraints. ER error lawsuits may also focus more on misdiagnosis due to the complexity of symptoms in emergency situations.